A challenging case - March 15, 2021
By Lorenzo Tavelli1,2 & Shayan Barootchi1,2, presented by Mario Romandini3
- Department of Periodontics & Oral Medicine, University of Michigan School of Dentistry, Ann Arbor, MI, USA
- Center for clinical research and evidence synthesis in oral tissue regeneration (CRITERION)
- ETEP (Etiology and Therapy of Periodontal and Peri-implant Diseases) Research Group, University Complutense, Madrid, Spain
When Prof. Filippo Graziani invited me to coordinate a clinically-oriented section of the Periocampus Herald, I felt that the “PerioArena” should be a space for the most talented young clinicians to present and discuss challenging clinical cases. Accordingly, the vision of the PerioArena is to provide to the reader not only the results of the treatment, which of course are expected to be excellent, but also and especially the surgical tips and secrets on how such results are reproducible in the day-to-day clinical practice.
If the goal is to invite highly talented young clinicians, I believe that it may be considered fully achieved for this Volume of the Periocampus Herald. Indeed, in this PerioArena issue, I have the privilege to introduce a case report by Dr. Lorenzo Tavelli and Dr. Shayan Barootchi, particularly reknown for the incredible things they are carrying out for the Perio-World.
Despite his very young age (yes, he is only 29!), Lorenzo is already one of the most important soft tissue experts in the Perio-World. Indeed, he has combined incredible scientific results (with more than 50 publications in the last 3 years!) with refined clinical skills. Above all, he is a close friend for sure, and one of the positive surprises of my year 2020 (yes, also a lot of good things happened in 2020…) And for what it’s worth, he also happens to be a Juventus fan!
While I have not had the chance to meet Shayan personally,
In this PerioArena, Lorenzo and Shayan present the elegant management of peri-implant soft tissue dehiscence, a clinical problem which is becoming a hot topic in our field. They will probably be two of the future leading experts on this topic. Indeed, among several other projects, they are currently completing the first-ever randomised clinical trial on soft-tissue dehiscence around dental implants. For this reason, you will also enjoy the detailed introduction and discussion they prepared to accompany the clinical case. At the end of their case report, you will find a brief “Question and Answer” section to get an even better insight into their case’s details. Let us start by taking a look at this beautiful case!
ABSTRACT
The treatment of peri-implant soft tissue dehiscence (PSTD) can be quite challenging for many clinicians, and leave gravely disappointing esthetic remarks for patients to bear.
The present report describes the treatment of such esthetic complication in the forefront of the anterior region, with the combined surgical-prosthetic approach. The patient had previously been provided with the option of implant explantation.
The initially deep positioned implant-supported crown was removed to allow for soft tissue expansion over a period of four weeks, followed by horizontal and vertical soft tissue augmentation using autogenous grafts to allow for the most predictable increase in keratinised mucosa width and thickness. The next stage included a prosthetic phase in which the patient received a newly fabricated crown and anterior veneers for the adjacent anterior teeth.
This report highlights the importance of proper diagnosis and treatment planning of such scenarios and the crucial interplay of a multidisciplinary treatment approach for achieving optimum results. Lastly, a novel esthetic score (Implant soft tissue Dehiscence coverage Esthetic Score – IDES), mainly to assess PSTD coverage, is utilised to evaluate and describe our esthetic outcomes.
1. Risk factors for peri-implant soft tissue dehiscences
There is no doubt that implant therapy is a predictable and reliable option for replacing missing dentition or hopeless teeth. Nonetheless, several biologic- and prosthetic-related complications are known to occur due to or concomitant to implant therapy (Barootchi et al., 2020b). Among them, a peri-implant soft tissue dehiscence (PSTDs) is likely the most noticeable among patients (Zucchelli et al., 2020). Indeed, this condition is characterised by an implant-supported crown that is longer than its homologous natural tooth and/or by an apical shift of the soft tissues, revealing the implant components (Figure 1). These esthetic complications can impair patients’ perception of implant therapy and possibly leave a negative impact on their quality of life (Anderson et al., 2014, Zucchelli et al., 2019).

Figure 1. Peri-implant soft tissue dehiscences (PSTDs) in the esthetic region. A) Multiple PSTDs in the maxillary central incisors with exposure of the abutment. B) PSTD with a crown longer than the homologous tooth and with the abutment and implant fixture exposure. C) PSTD with a crown longer than the homologous tooth. D) PSTD with a crown longer than the homologous tooth and the concomitant exposure of the abutment.
Several risk factors for the occurrence of PSTDs have been identified, including an inadequate amount of keratinised mucosa and soft tissue thickness (Lin et al., 2013, Sanz-Martin et al., 2020), buccally positioned implants (Sanz-Martin et al., 2020), thin buccal bone (Monje et al., 2019), bony dehiscence or fenestrations (Hammerle and Tarnow, 2018) and multiple adjacent dental implants (Romandini et al., 2020, Sanz-Martin et al., 2020). Given all of these risk factors, it is not surprising that the incidence of PSTDs has been estimated at 26.1% at the individual level, and 12% at the implant level (Romandini et al., 2020).
While the onset of these risk factors may be prevented and/or managed during the implant placement or at the second stage/uncovering phase, there is still limited evidence on the impact of these parameters on PSTD treatment outcomes. It can be speculated that augmentation of the peri-implant soft tissues, in terms of keratinised mucosa width and mucosal thickness, can sufficiently compensate implant malpositioning, thin buccal bone or bone dehiscence/fenestration. Nevertheless, randomised clinical trials and long-term studies in this regard are missing. It is reasonable to assume that the goals of PSTD treatment should be:
- Correction of the soft tissue defect, meaning, the soft tissue margin coronally repositioned at the level of the homologous natural tooth
- Recreation of an adequate dimension of peri-implant soft tissues (keratinised mucosa width and mucosal thickness)
- Patient satisfaction
2. Treatment approaches for the treatment of peri-implant soft tissue dehiscences
Several approaches have been described for the treatment of PSTDs, including the coronally advanced flap in combination with a connective tissue graft, the tunnel technique, the VISTA approach, free gingival grafts, guided bone regeneration procedures, the resubmergence technique, the surgical-prosthetic approach and the connective tissue graft-platform approach (Anderson et al., 2014, Burkhardt et al., 2008, Mazzotti et al., 2018, Stefanini et al., 2020, Zucchelli et al., 2013).
The indication for these techniques largely depends on the characteristics of the PSTD, which includes the height of the implant-supported crown, the buccolingual position of the implant and the dimension of the papillae.
Our group recently introduced a classification for PSTDs, together with recommendations for their treatment (Zucchelli et al., 2019). Four major classes (I, II, III and IV) were identified based on the buccolingual position of the implant crown/platform, with three subclasses (a, b and c) that relate to the height of the peri-implant papillae (Table 1).
While “traditional” approaches may successfully be employed for treating class Ia or IIa PSTDs (when the implant crown has the same height as of its homologous natural tooth), in the case of shallow or flat peri-implant papillae, the removal of the implant-supported crown is required along with more complex surgical approaches including a multidisciplinary workflow with a prosthodontist.
In the present article, we describe the treatment of a class IIIa PSTD using the combined surgical-prosthetic approach.
Table 1. Characteristics of patients at baseline and ultrasonographic analysis at the implant sites (Zucchelli et al., 2019).
|
Class |
Peri-implant soft tissue dehiscence/deficiency characteristics |
|
I |
The soft tissue margin is located at the same level of the ideal position of the gingival margin of the homologous natural tooth, and the color of the abutment/implant is visible only through the mucosa and/or there is a lack of keratinised tissue/soft tissue thickness |
|
II |
The soft tissue margin is located more apical to the ideal position of the gingival margin of the homologous natural tooth, and the implant-supported crown profile is located inside (more palatal) the imaginary curve line that connects the profile of the adjacent teeth at the level of the soft tissue margin |
|
III |
|
|
IV |
|
|
Subclass |
|
|
a |
|
|
b |
|
|
c |
The height of at least one papilla is <1 mm coronal to the ideal position of the soft tissue margin of the implant-supported crown |
3. Case presentation and management
A 24-year old systemically and periodontally healthy woman presented to the Graduate Periodontics Clinic at the School of Dentistry, University of Michigan, with the chief complain of poor esthetics of her maxillary left central incisor’s implant crown (Figure 2).

Figure 2. PSTD at baseline. The patient mentioned that the implant-supported crown had been modified over the years with the addition of pink porcelain
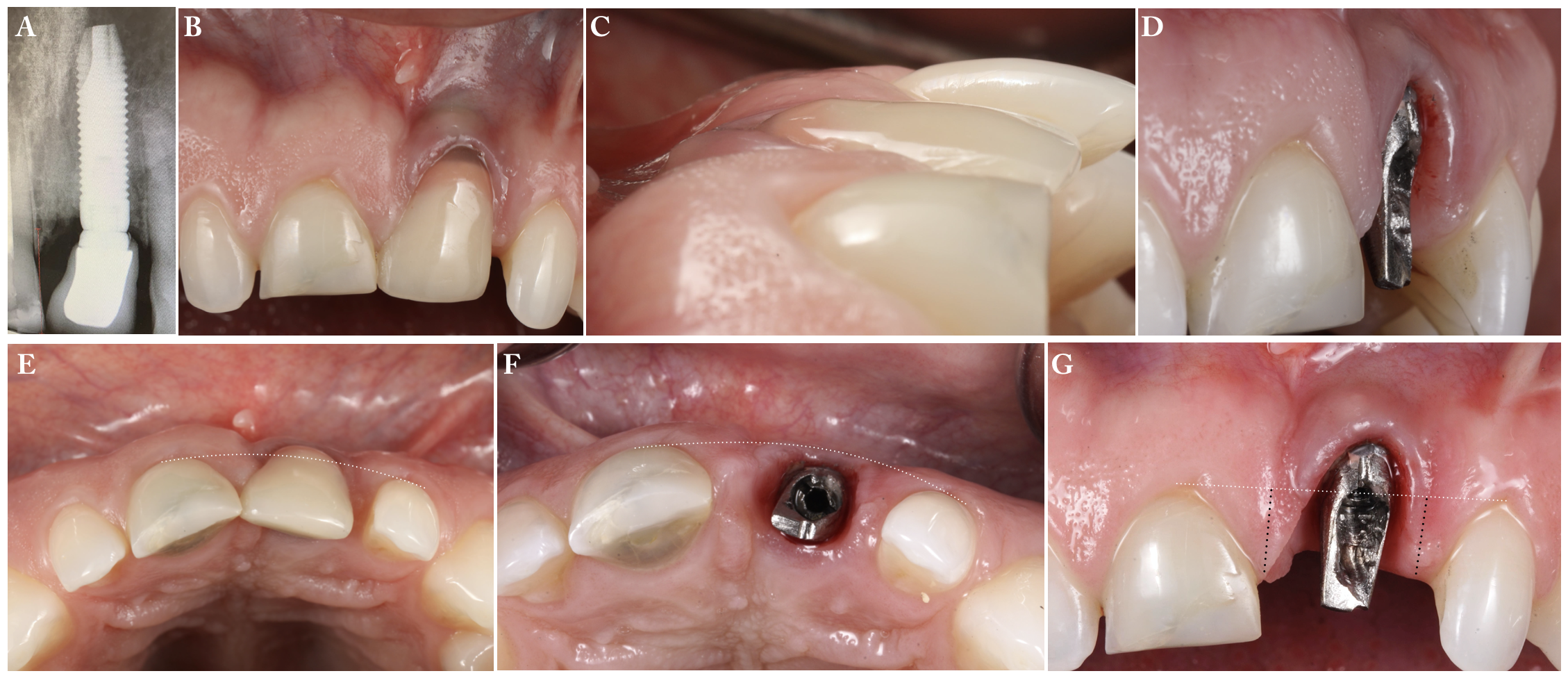
Figure 3. A) Peri-apical x-ray. B) Frontal view of the PSTD. C) Lateral view of the PSTD. D) Lateral view of the PSTD after crown removal. E) Occlusal view showing that the implant-supported crown is more buccal than the imaginary line connecting the two adjacent teeth. At that point, the PSTD can be class III or IV. After crown removal, f) Occlusal view shows that the implant platform is within the imaginary line connecting the two adjacent teeth. The PSTD is classified as class III. G) Frontal view of the PSTD showing the peri-implant papillae height (black dotted lines). Both papillae are ≥ 3 mm in height, and therefore the subclass of the PSTD is “a”.
3.1 Presurgical phase
Oral hygiene instructions were reviewed and reinforced 6 weeks before the surgical visit. The implant-supported crown was removed 1 month before the surgical phase, followed by recontouring the underlying abutment. The temporary crown was prepared shorter than the previous crown and approximately 2 mm away from the peri-implant soft tissues (Figure 4).

Figure 4. A) Frontal view of the PSTD after crown removal. B) A “short” provisional crown was fabricated and cemented to the abutment and adjacent teeth to leave more space for the soft tissue to grow before the surgical procedure. C) Frontal view of the PSTD at the day of the surgical procedure. It is possible to appreciate the soft tissue volume gain that occurred after removing the previous crown.
3.2 Surgical procedure
The presurgical phase allowed the soft tissues to grow and fill the previously occupied space by the crown, leading to an increase in height, width, and thickness of interproximal soft tissues (Figure 5A). After removing the provisional crown, a trapezoidal-shape coronally advanced flap was performed (Figure 5B). The distance between the baseline position of the buccal soft tissue margin and its ideal final position is the reference for tracing the horizontal incisions of the coronally advanced flap, starting from the most palatal aspect of the papilla. Then, two slightly divergent bevelled oblique incisions were placed and extended to the alveolar mucosa.

Figure 5. A) Frontal view of the PSTD after the removal of the temporary crown. B) Design of the coronally advanced flap with two oblique vertical incisions.
A split-thickness flap was elevated, with meticulous attention paid to separate and leave the overlying flap’s connective tissue on the implant surface, without completely removing it (Figure 6A). Maintaining this layer of attached connective tissue on the implant threads is an important step that differentiates flap elevation on healthy implants with PSTDs from implant with peri-implantitis.
The flap was released with a deep incision parallel to the bone and then with a superficial incision with the blade parallel to the external mucosal surface. The flap was able to passively reach a position 2 mm coronal to the soft tissue margin’s ideal position. The anatomical papillae were de-epithelialised with a microblade, not only on the buccal aspect but also in the occlusal region to enhance the vascular bed for the flap.
A free gingival graft of approximately 10 mm in width, 5 mm in height and 2 mm in thickness was harvested from the palate and then extra-orally de-epithelialised to obtain a dense and fibrous connective tissue graft. A collagen sponge was applied to the palatal donor site and stabilised with 5/0 vicryl cross-sutures. A thin layer of cyanoacrylate tissue glue was applied on top of the collagen sponge, as previously described (Tavelli et al., 2019c, Tavelli et al., 2018) (Figure 6 B-E).
No chemical or mechanical root conditioning agent was applied on the implant surface. However, to allow for a better adaptation and blood supply of the connective tissue graft during the healing, a light recontouring of the abutment was performed before the stabilisation of the graft.
The connective tissue graft was stabilised with simple interrupted sutures (5/0 chromic gut) to the de-epithelialised anatomical papillae on the coronal aspect and to the periosteum on its apical portion. The graft was further adapted to the recipient bed with a compressive suture (5/0 chromic gut) (Figure 6B).
The flap was sutured 2 mm coronal to the soft tissue margin’s ideal final position by performing simple interrupted sutures at the level of the vertical releasing incisions and sling sutures around the abutment. Simple interrupted sutures were also placed between the surgical and the anatomical papillae for promoting a better adaptation of the soft tissues and a healing by primary intention (Figure 6A). A short temporary crown was cemented onto the abutment and the adjacent teeth in a way to avoid any contact with the coronally positioned soft tissues (Figures 6B).

Figure 6. A) Flap elevation. It is possible to appreciate that several threads of the implant are outside the buccal bone with a thin layer of connective tissue attachment that was left in place during the flap elevation. B) Stabilisation of the connective tissue graft to the recipient site. C-D) Dimension of the connective tissue graft. E) A collagen sponge was sutured on the palatal donor site and further stabilised with a layer of cyanoacrylate tissue glue.
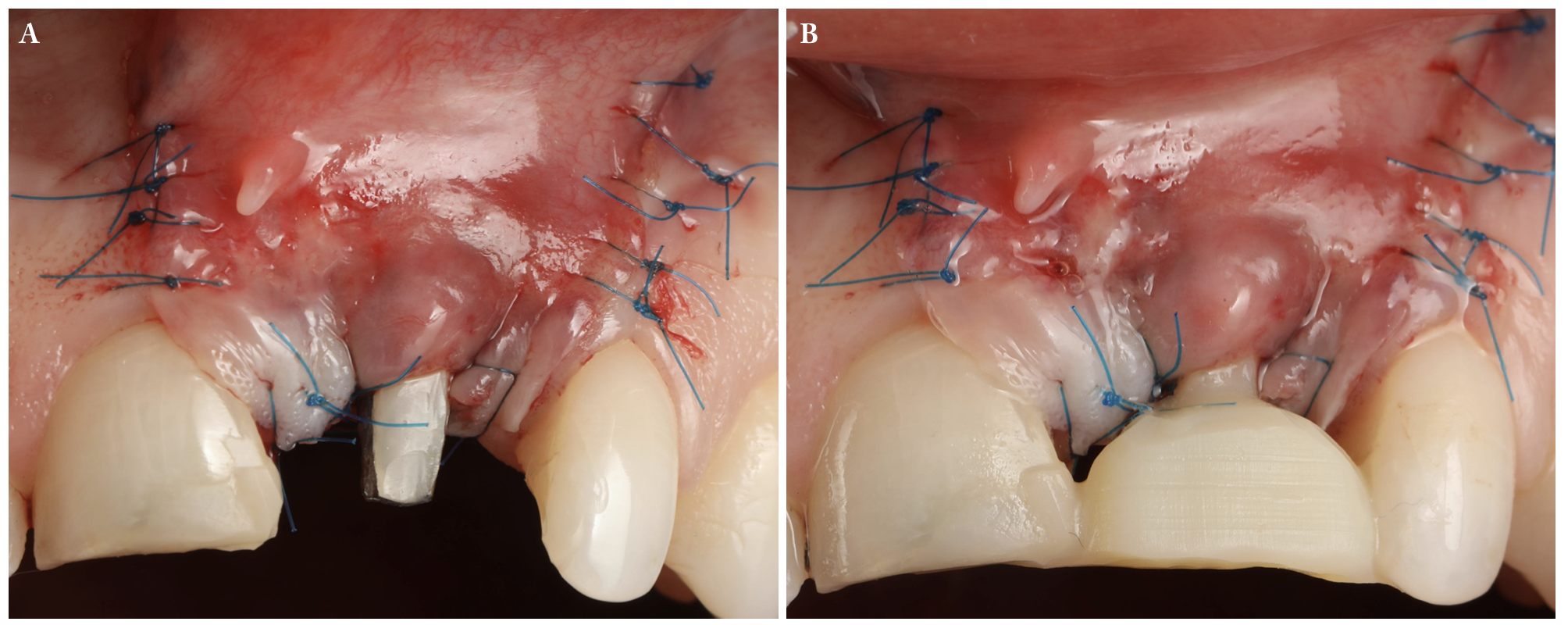
Figure 7. A) Suturing of the coronally advanced flap. Simple interrupted sutures from the flap to the adjacent soft tissue engaging the periosteum were performed at the vertical releasing incisions level. A combination of sling sutures and simple interrupted sutures was performed at the surgical papillae level, engaging the anatomical de-epithelialised papillae and the occlusal/palatal soft tissue. B) The temporary crown was readapted and cemented to the abutment and the adjacent soft tissue in a way that contacts with the flap were avoided.
3.3 Post-surgical phase
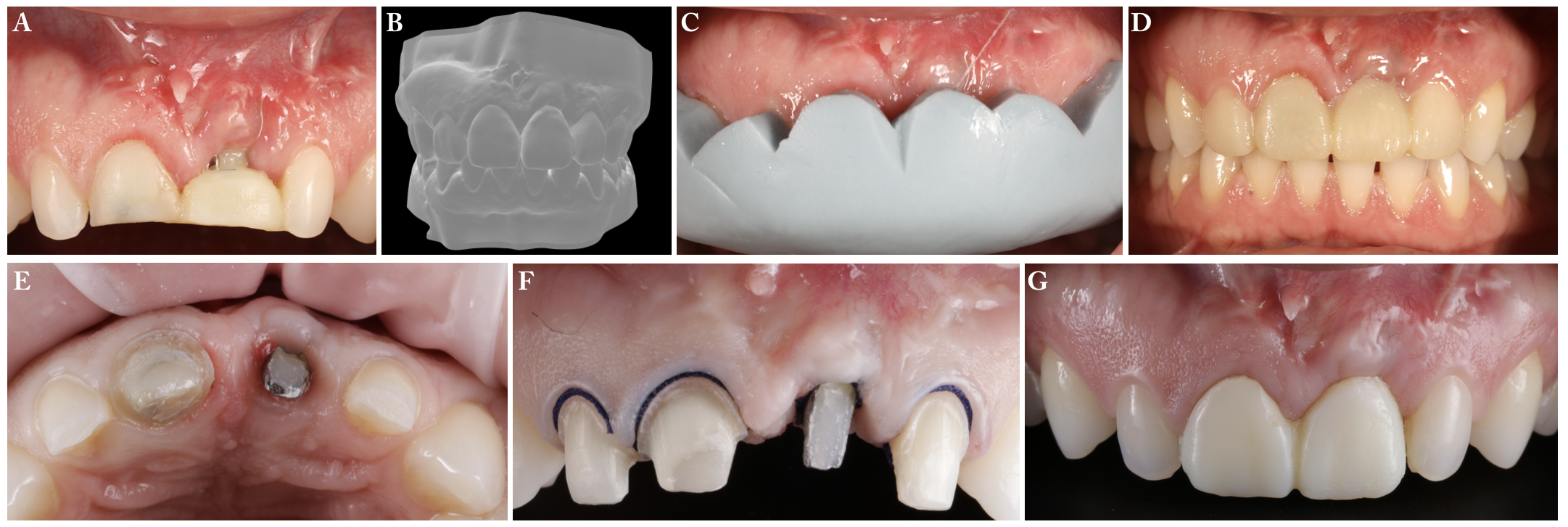
Figure 8. A) Healing at 3 months. B) Digital wax-up. C-D) Intraoral trying of the wax-up. E-G) Preparation of the crown on the right maxillary incisor and the veneers on the maxillary lateral incisors at the 9-month follow-up.
Five months after the surgical procedure, a digital wax-up was performed to design a new crown on the right maxillary central incisor and two veneers for the lateral incisors (Figure 8). Ten months after the surgical procedure, the final restorations were delivered (Figure 9).
4. 1-year outcomes
At the 1-year follow-up visit, the patient presented with a complete coverage of the previous PSTD (Figures 9 and 10). The KTW increased from 2.5 mm to 3.5 mm. The mucosal thickness changes were evaluated from the superimposition of digital intraoral impressions (3D analysis) and ultrasonography scans (Figure 10). The initial mucosal thickness, measured 1.5 mm and 3.5 mm below the soft tissue margin, was 0.73 mm and 0.78 mm, respectively. After 1 year, the mucosal thickness was 2.23 mm and 2.74 mm when measured by 1.5 mm and 3.5 mm below the soft tissue margin. The mucosal thickness gain amounted to 1.5 mm, and 1.96 mm, respectively.
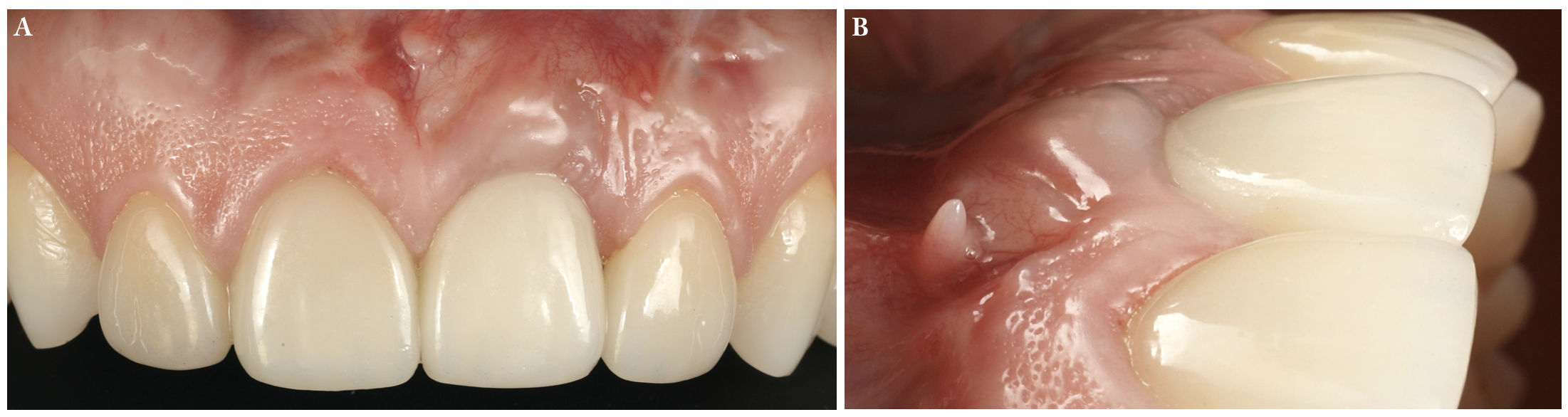
Figure 9. 1-year outcome. It is possible to appreciate the complete coverage of the soft tissue dehiscence in the frontal view (A), with the soft tissue margin positioned at the right central incisor’s same level. The lateral view (B) shows the significant soft tissue volume gain achieved.
Linear dimensional changes obtained from the superimposition of intraoral digital impressions at baseline and at the 1-year follow-up ranged between 1.16 mm and 1.53 mm, further demonstrating a substantial increase in the buccal soft tissue thickness (Figure 10).
The patient expressed great satisfaction with the treatment, mentioning that the final outcome was “life-changing”.
In addition, the professional esthetic result was evaluated with a novel score, specifically designed and introduced to yield the Implant soft tissue Dehiscence coverage Esthetic Score (IDES) (Zucchelli et al., 2021) (Table 2). Five points (maximum) were assigned for the soft tissue margin position, and 3 points (maximum) were given to the height of the peri-implant papillae. The colour of the peri-implant mucosa was noticeably different and distinguishable from the adjacent soft tissues, therefore, 0 points were assigned to the parameter of “Peri-implant Mucosa”, and due to the small scar that was apparent on the distal aspect of the implant crown’s peri-implant mucosa, a score of 0 was also assigned for the category of “Peri-implant Mucosa Appearance”.
Therefore, the final score was summed up to 8 out of the total 10 points achievable on the IDES rubric.

Figure 10. Clinical-, 3D digital volumetric- and ultrasonographic- comparison of the 1-year and baseline time points. A) Frontal view at baseline. B) Frontal view at the 1-year follow-up. C) Digital intraoral impressions were taken with a digital scanner (3Shape Trios, 3Shape, Denmark) and imported as STL files in a specific software (GOM Inspect, Zeiss Company, Germany) for the superimposition (Tavelli et al., 2021). The linear dimensional changes between baseline (BL) and the 1-year follow-up (1y) are shown. D) Lateral view at baseline. E) Lateral view at the 1-year follow-up. F) Ultrasonographic evaluation of the peri-implant phenotype at the 1-year follow-up. It is possible to appreciate the implant-supported crown (C), the abutment (A), the implant threads (I) and the soft tissue (ST). The mucosal thickness evaluated 1.5 mm below the soft tissue margin was 2.225 mm, while the mucosal thickness assessed 3.5 mm and 5.5 mm below the soft tissue margin were 2.738 mm and 2.523 mm, respectively.
Table 2. Peri-implant soft tissue Dehiscence coverage Esthetic Score (IDES) (Zucchelli et al., 2021)
|
Peri-Implant soft tissue Dehiscence coverage Esthetic Score (IDES) |
||
|
Parameter (points) |
Condition at least 6 months after treatment |
Assigned points |
|
Soft Tissue Margin (STM) (0-5) |
No improvement of the PSTD |
0 |
|
Partial coverage of the PSTD but the metallic components are still visible |
1 |
|
|
Complete coverage of the metallic components (or abutment) only, but the implant-supported crown is still longer than the homologous tooth |
2 |
|
|
Complete coverage of the metallic components with the mucosal margin at the same level of the homologous tooth |
5 |
|
|
Peri-implant papillae height (PPH) (0-3) |
Both papillae are more apical than the healthiest papilla tip of the homologous tooth |
0 |
|
Only one papilla is at the same level (or more coronal) of the healthiest papilla tip of the homologous tooth |
1 |
|
|
Both papillae are at the same level (or more coronal) of the healthiest papilla tip of the homologous tooth |
3 |
|
|
Peri-implant Mucosa Color (PMC) (0-1) |
Distinguishable from the adjacent soft tissue |
0 |
|
Not distinguishable from the adjacent soft tissue |
1 |
|
|
Peri-implant Mucosa Appearance (PMA) (0-1) |
Presence of at least one of these conditions: scar tissue, MGJ not-aligned, tissue volume too thin or too thick compared to the adjacent soft tissue or tissue texture not similar to the adjacent soft tissue |
0 |
|
Absence of scar tissue, MGJ well aligned, tissue volume in line with the adjacent soft tissue or tissue texture similar to the adjacent soft tissue |
1 |
|
5. Discussion
A large body of evidence supports the efficacy of coronally advanced flap + connective tissue graft for treating gingival recessions (Tavelli et al., 2019a, Barootchi et al., 2020c). However, when the same “traditional” technique is applied to recession defects at implant sites (PSTDs), the outcomes are not as predictable or satisfactory as can be expected with natural teeth (Anderson et al., 2014). In a randomised clinical trial on consecutively enrolled and treated patients, Anderson and coworkers evaluated the efficacy of coronally advanced flap with its traditional design as commonly performed around teeth, involving two vertical releasing incisions and the addition of either a connective tissue graft (harvested from the deep palate) or an acellular dermal matrix. The study observed a mean PSTD coverage of 40% for coronally advanced flap + connective tissue graft, and 28% for coronally advanced flap + acellular dermal matrix. The limited amount of recession coverage was also conveyed by the patients’ self-reported esthetics that did not improve 6 months after the treatment (Anderson et al., 2014). In a pilot study, Burkhardt et al. included ten patients presenting isolated PSTDs with unrestored contralateral teeth for comparison (Burkhardt et al., 2008). The PSTDs were treated with coronally advanced flap and a subepithelial connective tissue graft with a coronally positioned flap with an average overcompensation of 1.2 mm. Over time, the authors observed a shrinkage of the soft tissues with a mean PSTD coverage of 75% at 1 month, and 70% at 3 months. The final mean PSTD was 66% at the 6-month follow-up, with none of the sites showing complete PSTD coverage. The authors suggested that the lack of a periodontal ligament and the overall reduced blood supply of the peri-implant tissues may be one of the factors that may have negatively impacted the outcomes (Burkhardt et al., 2008).
Zucchelli and coworkers demonstrated that crown removal at least one month before the surgical procedure can improve coronally advanced flap predictability at implant sites (Zucchelli et al., 2013). Indeed, the increased soft tissue volume after crown removal and the possibility of advancing the flap also on the occlusal aspect play a crucial role in the early wound healing of the flap. On the other hand, maintaining the crown during the surgical procedure, especially when the peri-implant papillae are shallow, may impair the surgical papillae’s blood supply, with an increased chance of significantly shrinking the flap. In addition, the use of a connective tissue graft derived from the most superficial layer of the palate may have also contributed to the significant volumetric gain observed in this case (1.5-1.96 mm). As a subepithelial connective tissue graft from the deep palate contains more fatty and glandular tissues, it may limit the amount of gain in mucosal thickness and may cause a higher shrinkage of the graft/soft tissues (Zucchelli et al., 2010, Zucchelli et al., 2020, Tavelli et al., 2020b).
PSTD treatment outcomes should also be evaluated in terms of changes in the peri-implant soft tissue phenotype. Indeed, only a thick, soft tissue thickness with an adequate band of keratinised mucosa can prevent the reoccurrence of the soft tissue defect. The beneficial role of gingival thickness on the gingival margin’s stability has been demonstrated in natural dentition (Barootchi et al., 2020c, Tavelli et al., 2019b). At implant sites, the only long-term outcomes of PSTD treatment have been published by Zucchelli and coworkers that show stable results up to 5 years (Zucchelli et al., 2018). A recent network meta-analysis from our group further demonstrated the beneficial effects of mucosal thickness augmentation on marginal bone levels’ stability. In addition, it was also found that keratinised mucosa augmentation contributed to peri-implant health (Tavelli et al., 2020a).
In this view, novel and non-invasive technologies such as optical scanning and ultrasonography to evaluate the peri-implant phenotype and its changes are beneficial and well accepted by patients (Tavelli et al., 2021, Barootchi et al., 2020a, Chan and Kripfgans, 2020).
Lastly, it should be observed that although PSTD treatment is mainly focused on improving esthetic concerns, a specific index evaluating the esthetic outcomes following the surgical correction of PSTDs was missing in the literature. Previous studies utilised visual analogue scales or indices proposed for implant therapy, such as the complex esthetic index, and the pink, or white esthetic scores. Our group recently suggested the utilisation of IDES to assess the esthetic outcome of PSTD treatment, which showed high reproducibility in results among periodontists and between multiple time points (Zucchelli et al. In the case presented within this article, the maximum scores were assigned to the categories of and for the position of the soft tissue margin, as well as the height of the papillae. However, the colour and the appearance of the peri-implant mucosa exhibited discrepancies relative to the adjacent soft tissues, and both received a score of zero on their scale. Indeed, obtaining a “perfect” esthetic result when treating PSTDs is challenging, as one of the main setbacks of this path is the very nature of the peri-implant soft tissues, that relative to those of natural teeth, resemble a pattern of healing by scar formation. Future studies are required to reveal and explore the factors contributing to the final peri-implant mucosa colour and its texture.
6. Conclusions
Peri-implant soft tissue dehiscences in the esthetic area are not rare findings. Correct diagnosis and treatment planning are crucial for the correction of this condition. The present case depicts the treatment of peri-implant soft tissue dehiscence with the combined surgical-prosthetic approach. One year after the treatment, a complete resolution of the defect was observed together with a modification of the peri-implant soft tissue phenotype and satisfactory esthetic outcomes.
Conflict of interest:
“Question & Answer” section
(Mario questions and Lorenzo & Shayan answer)
- Do you think that, in the context of a surgical-prosthetic approach for treating PSTD, other surgical options (e.g., tunnelling) may be considered as equally-effective alternatives to coronally advanced flap?
It really depends on the type of PSTD. It is mandatory to remove the crown of an implant with PSTD when the clinical crown is longer than the homologous natural tooth because otherwise there are almost no chances for the flap to survive when coronally repositioned. In addition, the height and the width of the peri-implant papillae are also crucial factors to take into consideration when choosing the most appropriate surgical approach. If the papillae are too shallow or too narrow (usually due to the crown occupying most of the interproximal space), the flap has a high risk of necrosis/dehiscence. Crown removal at least 1 month before the surgical procedure results in an increased interproximal soft tissue volume, which facilitates the execution and improves the outcomes of coronally advanced flap, either with or without vertical releasing incisions. PSTDs with flat papillae (subclass c) require more complex approaches, involving multiple soft tissue grafts and a submerge healing.
Tunnel technique has limited indications for the treatment of PSTDs, such as PSTDs with an adequate crown height and papillae dimensions. However, it has to be considered that the peri-implant soft tissue tends to be more fragile and also more challenging to elevate compared to natural teeth. In our experience, tunnel technique is not as predictable as a coronally advanced flap in these scenarios.
- Can you make a confidence to our readers about some technical tips for managing peri-implant soft-tissue dehiscence cases like this one?
We believe that a careful case planning is the key to treating PSTDs. The clinician should not “rush” to perform the surgical procedure since a collaboration with the prosthodontic is often necessary. Complex cases may also involve the restoration of the adjacent natural teeth with crowns or veneers. During the surgery, we recommend executing a split-thickness flap in the area of the implant to preserve the attachment of the connective tissue fibres of the flap to the (healthy and not-contaminated) implant surface. The connective tissue graft dimensions should be slightly “bigger” compared to the grafts usually harvested for root coverage procedures in natural dentition. Due to the reduced vascularisation of the implant site compared to the periodontium, a higher shrinkage of the graft may be expected. Lastly, the management of the temporary crowns during the early and late phases of the healing is crucial for achieving a satisfactory esthetic result.
LITERATURE AND SUGGESTED READS
Anderson, L. E., Inglehart, M. R., El-Kholy, K., Eber, R. & Wang, H. L. (2014) Implant associated soft tissue defects in the anterior maxilla: a randomised control trial comparing subepithelial connective tissue graft and acellular dermal matrix allograft. Implant Dent 23, 416-425. doi:10.1097/ID.0000000000000122.
Barootchi, S., Chan, H. L., Namazi, S. S., Wang, H. L. & Kripfgans, O. D. (2020a) Ultrasonographic characterisation of lingual structures pertinent to oral, periodontal, and implant surgery. Clin Oral Implants Res 31, 352-359. doi:10.1111/clr.13573.
Barootchi, S., Ravida, A., Tavelli, L. & Wang, H. L. (2020b) Nonsurgical treatment for peri-implant mucositis: A systematic review and meta-analysis. Int J Oral Implantol (Berl) 13, 123-139.
Barootchi, S., Tavelli, L., Zucchelli, G., Giannobile, W. V. & Wang, H. L. (2020c) Gingival phenotype modification therapies on natural teeth: A network meta-analysis. J Periodontol 91, 1386-1399. doi:10.1002/JPER.19-0715.
Burkhardt, R., Joss, A. & Lang, N. P. (2008) Soft tissue dehiscence coverage around endosseous implants: a prospective cohort study. Clin Oral Implants Res 19, 451-457. doi:10.1111/j.1600-0501.2007.01497.x.
Chan, H. L. & Kripfgans, O. D. (2020) Ultrasonography for diagnosis of peri-implant diseases and conditions: a detailed scanning protocol and case demonstration. Dentomaxillofac Radiol, 20190445. doi:10.1259/dmfr.20190445.
Hammerle, C. H. F. & Tarnow, D. (2018) The etiology of hard- and soft-tissue deficiencies at dental implants: A narrative review. J Clin Periodontol 45 Suppl 20, S267-S277. doi:10.1111/jcpe.12955.
Lin, G. H., Chan, H. L. & Wang, H. L. (2013) The significance of keratinised mucosa on implant health: a systematic review. J Periodontol 84, 1755-1767. doi:10.1902/jop.2013.120688.
Mazzotti, C., Stefanini, M., Felice, P., Bentivogli, V., Mounssif, I. & Zucchelli, G. (2018) Soft-tissue dehiscence coverage at peri-implant sites. Periodontol 2000 77, 256-272. doi:10.1111/prd.12220.
Monje, A., Chappuis, V., Monje, F., Munoz, F., Wang, H. L., Urban, I. A. & Buser, D. (2019) The Critical Peri-implant Buccal Bone Wall Thickness Revisited: An Experimental Study in the Beagle Dog. Int J Oral Maxillofac Implants 34, 1328-1336. doi:10.11607/jomi.7657.
Romandini, M., Pedrinaci, I., Lima, C., Costanza Soldini, M., Araoz, A. & Sanz, M. (2020) Prevalence and risk/protective indicators of buccal soft tissue dehiscence around dental implants. J Clin Periodontol. doi:10.1111/jcpe.13417.
Sanz-Martin, I., Regidor, E., Navarro, J., Sanz-Sanchez, I., Sanz, M. & Ortiz-Vigon, A. (2020) Factors associated with the presence of peri-implant buccal soft tissue dehiscences: A case-control study. J Periodontol. doi:10.1002/JPER.19-0490.
Stefanini, M., Marzadori, M., Tavelli, L., Bellone, P. & Zucchelli, G. (2020) Peri-implant Papillae Reconstruction at an Esthetically Failing Implant. Int J Periodontics Restorative Dent 40, 213-222. doi:10.11607/prd.4296.
Tavelli, L., Asa’ad, F., Acunzo, R., Pagni, G., Consonni, D. & Rasperini, G. (2018) Minimising Patient Morbidity Following Palatal Gingival Harvesting: A Randomized Controlled Clinical Study. Int J Periodontics Restorative Dent 38, e127-e134. doi:10.11607/prd.3581.
Tavelli, L., Barootchi, S., Avila-Ortiz, G., Urban, I. A., Giannobile, W. V. & Wang, H. L. (2020a) Peri-implant soft tissue phenotype modification and its impact on peri-implant health: A systematic review and network meta-analysis. J Periodontol. doi:10.1002/JPER.19-0716.
Tavelli, L., Barootchi, S., Cairo, F., Rasperini, G., Shedden, K. & Wang, H. L. (2019a) The Effect of Time on Root Coverage Outcomes: A Network Meta-analysis. J Dent Res 98, 1195-1203. doi:10.1177/0022034519867071.
Tavelli, L., Barootchi, S., Di Gianfilippo, R., Modarressi, M., Cairo, F., Rasperini, G. & Wang, H. L. (2019b) Acellular dermal matrix and coronally advanced flap or tunnel technique in the treatment of multiple adjacent gingival recessions. A 12-year follow-up from a randomised clinical trial. J Clin Periodontol 46, 937-948. doi:10.1111/jcpe.13163.
Tavelli, L., Barootchi, S., Majzoub, J., Siqueira, R., Mendonca, G. & Wang, H. L. (2021) Volumetric changes at implant sites: A systematic appraisal of traditional methods and optical scanning-based digital technologies. J Clin Periodontol 48, 315-334. doi:10.1111/jcpe.13401.
Tavelli, L., Barootchi, S., Namazi, S. S., Chan, H. L., Brzezinski, D., Danciu, T. & Wang, H. L. (2020b) The influence of palatal harvesting technique on the donor site vascular injury: A split-mouth comparative cadaver study. J Periodontol 91, 83-92. doi:10.1002/JPER.19-0073.
Tavelli, L., Ravida, A., Saleh, M. H. A., Maska, B., Del Amo, F. S., Rasperini, G. & Wang, H. L. (2019c) Pain perception following epithelialised gingival graft harvesting: a randomised clinical trial. Clin Oral Investig 23, 459-468. doi:10.1007/s00784-018-2455-5.
Zucchelli, G., Barootchi, S., Tavelli, L., Stefanini, M., Rasperini, G. & Wang, H. L. (2021) Implant soft tissue Dehiscence coverage Esthetic Score (IDES): A pilot within- and between-rater analysis of consistency in objective and subjective scores. Clin Oral Implants Res. doi:10.1111/clr.13706.
Zucchelli, G., Felice, P., Mazzotti, C., Marzadori, M., Mounssif, I., Monaco, C. & Stefanini, M. (2018) 5-year outcomes after coverage of soft tissue dehiscence around single implants: A prospective cohort study. Eur J Oral Implantol 11, 215-224.
Zucchelli, G., Mazzotti, C., Mounssif, I., Mele, M., Stefanini, M. & Montebugnoli, L. (2013) A novel surgical-prosthetic approach for soft tissue dehiscence coverage around single implant. Clin Oral Implants Res 24, 957-962. doi:10.1111/clr.12003.
Zucchelli, G., Mele, M., Stefanini, M., Mazzotti, C., Marzadori, M., Montebugnoli, L. & de Sanctis, M. (2010) Patient morbidity and root coverage outcome after subepithelial connective tissue and de-epithelialised grafts: a comparative randomised-controlled clinical trial. J Clin Periodontol 37, 728-738. doi:10.1111/j.1600-051X.2010.01550.x.
Zucchelli, G., Tavelli, L., McGuire, M. K., Rasperini, G., Feinberg, S. E., Wang, H. L. & Giannobile, W. V. (2020) Autogenous soft tissue grafting for periodontal and peri-implant plastic surgical reconstruction. J Periodontol 91, 9-16. doi:10.1002/JPER.19-0350.
Zucchelli, G., Tavelli, L., Stefanini, M., Barootchi, S., Mazzotti, C., Gori, G. & Wang, H. L. (2019) Classification of facial peri-implant soft tissue dehiscence/deficiencies at single implant sites in the esthetic zone. J Periodontol 90, 1116-1124. doi:10.1002/JPER.18-0616.
