Surgical Perspectives - January 10, 2022
The Modified Widman flap represents a historical milestone in the development of periodontal surgery as we know it. It has been proposed in that very active period - the intersection between the historical resective approaches and the regenerative procedures that would have been proposed in the early 80s. Given its historical relevance, many trainees are hearing this enigmatic flap numerous times during their studies but what everyone really craves to ask, but never dares, is: “Who was Widman? Who modified that??”
Why was surgical therapy even thought of in the first place?!
Historically, periodontal surgery was firstly proposed in order to reach what was the wildest daydream of any Periodontist born in the late 1800s: pocket elimination. Just afterwards, many periodontists, including Mr Widman himself, a widely renowned dentist within Sweden and, of course, within this issue of the Herald, highlighted the importance of what he called “competent root planing” for a successful periodontal therapy. As a consequence, all the sharpest surgical minds at the time came up with procedures aiming to facilitate the removal of subgingival calculus, as well as the hostile chronic inflammatory tissue that, on the other hand, was the wildest nightmare of any Periodontist born in the late 1800s.
The Original Widman flap
Who did it first? – The Gossip
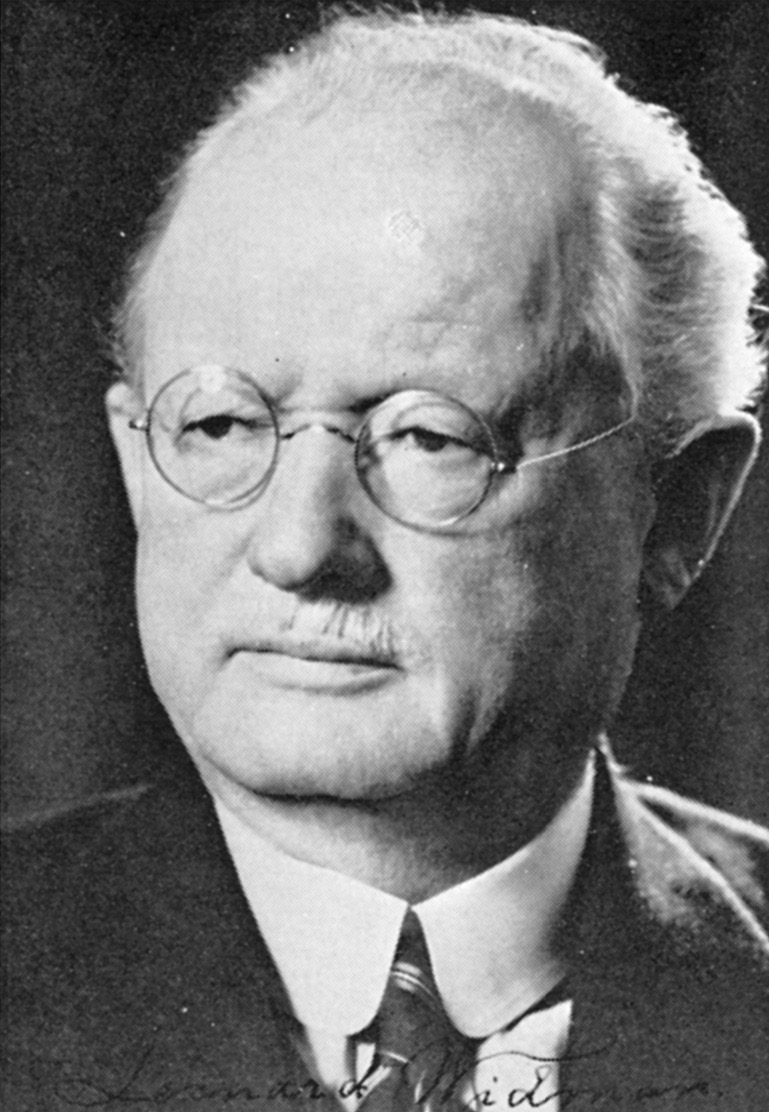
Our dear friend Mr Leonard Widman, whose portrait you can admire in Figure 1, proposed right at the end of the Second World War, in 1918, his article “The operative treatment of pyorrhea alveolaris: a new surgical method”. In this article, written entirely in Swedish and not translated into English, he firstly described the surgical procedure that goes by his name (i.e. the Widman flap). Unfortunately, this surgery, groundbreaking- to say the least- at the time, remained unknown for most part of Europe and the United States for many decades afterwards. In fact, it was not until Ake Widman, that is Leonard Widman’s son, published an article on the Journal of Periodontology (Everett et al., 1971) together with other two Perio giants, Frank G. Everett and Jens Waerhaug, that the real story behind the Widman flap came to light…
Ake Widman, from now on Widman Jr, supposedly came up with the idea to translate his father’s work few years after another Master of Perio, Friedman, proposed the Apically Positioned Flap to the scientific community (Friedman, 1962). From this paper, we can learn a lot about the technique but as much about its credit. In fact, as Widman Jr explained, in the early twenties of the last century, Europe was caught in two major crossfires: the first World war and the priority of this surgical procedure. So, while the whole world was busy thinking about the former, the world of Periodontists was there: struggling, debating, doubting and discussing about the latter (and, I must say, who are we to judge…). In fact, from Widman Jr words, we came to understand that at the time there was not just one, but two controversies regarding this flap! The first one was between Widman of Sweden and Neumann of Germany; the second one was between Zentler of the United States and Cieszynski of Poland, and the one didn’t know about the other… something unbelievable for the ever-connected world of today!
How did they do it?- The technique
In a nutshell, the Widman flap was a procedure characterized by a mucoperiosteal flap, whose aim was to remove the pocket epithelium and the inflamed connective tissue, hence facilitating the decontamination of the root surfaces.
We can summarize the procedure in 3 steps:
- Incisions: releasing incisions were used to delimitate the surgical field and were performed from the central part of the buccal gingival margin reaching beyond the mucogingival junction. The releasing incisions were then connected to a paramarginal incision following the profile of the free gingival margin. This incision allowed for the separation of the pocket epithelium and the inflamed connective tissue from the healthy gingival tissue.
- Flap elevation and tissue removal: the mucoperiosteal flap was then elevated in order to expose around 2-3mm of marginal alveolar bone. The inflamed pocket epithelium and connective tissue were removed and thus the root surface could be accessed to perform an accurate surgical debridement of the defects. In some cases, osteoplasty was also suggested.
- Flap repositioning: the buccal and oral flaps were then repositioned at the level of the alveolar bone crest with single interproximal sutures in order to achieve pocket elimination after surgery.
Why did they do it?- The perks
The Widman flap was proposed in a time (early 1900s) when the ordinary standard procedure to gain surgical access to root surfaces was the gingivectomy, that is the removal of the inflamed soft tissue of the pocket alone. While the aim of both procedures was pocket elimination, the gingivectomy aimed to eliminate pockets with a secondary intention healing (therefore, no sutures were placed), conversely with the Widman flap that included a primary intention healing. Therefore, the main advantages of the Widman flap compared to what was the gold standard procedure at the time were:
- less patient morbidity given that healing happened with primary intention;
- the possibility to perform osteoplasty in order to recreate a positive bone architecture.
The Modified Widman Flap
How did they do it?- The Technique
As if the controversies regarding the priority of the Widman flap were not enough, in 1974 Ramfjord and Nissle, that is the backbone of the Michigan School of Dentistry at the time, proposed in their article its modification, the so-called “Modified Widman flap” (Ramfjord & Nissle, 1974).
Again, we can summarize the procedure in 3 steps but please, focus on the lines of incisions (I’m going to tell you why later on…):
- Incisions (Figure 2B, Figure 2b): the first incision should be scalloped and paramarginal, parallel to the longitudinal axis of the tooth; it is usually performed around 1mm from the free gingival margin, depending on probing depth (if the buccal probing depth is <2mm it can be performed intrasulcular). If the incision was made paramarginal, the second incision should be intrasulcular reaching until the alveolar bone crest. Afterwards, the third incision should be horizontal at the basis of the secondary flap in order to facilitate its removal.
- Flap elevation and tissue removal (Figure 2C, Figure 2c): both buccal and oral flaps are full-thickness, but their elevation should be as minimal as possible in order to expose a maximum of 2-3mm of the alveolar bone crest. Once a direct access to the root surfaces is gained, the pocket epithelium and the granulation tissue are removed using mechanical instruments.
- Flap repositioning (Figure 2D, Figure 2d): both the buccal and oral flaps are repositioned at the level of the alveolar bone crest and in order to completely cover the interdental space. Flap adaptation can be facilitated by performing osteoplasty when necessary. Afterwards, flaps are fixated through single interrupted sutures in the interdental spaces.
Therefore, from the 3-step summaries that I kindly provided you with (no worries, you will thank me later), we can easily understand that the two procedures differ for the apical repositioning of the flap and the execution of bone remodeling in order to achieve pocket elimination (“Oh, what a dream!”, my 1970s-self would have thought).

Figure 2: shows the surgical phases from buccal (indicated with capital letters) and palatal side; A, a) pre-op; B, b) incision lines, with the blue arrow indicating the 1974 incision and the yellow arrow the 1977 modification; C, c) flap elevation; D, d) flap repositioning and sutures placement; E, e) one month post-op.
Why did they do it?- The perks
Of course if we compare the modified Widman flap with the original Widman flap it is clear, even for less experienced eyes, that the former, when compared to the latter, reduced patients morbidity due to the minimal flap elevation and also allowed for a minimal exposition of the root surfaces when compared to the Widman flap, thus gaining an aesthetic advantage. Nonetheless, the apical migration following this procedure was extremely consistent, thus leaving room for further aesthetic improvements…
The “modified” Modified Widman Flap
Who modified that??- The Gossip
Just when you thought you knew it all about the modified Widman flap, Ramfjord in 1977 proposed a further modified version of the already modified Widman flap. Actually, if we go through his work, we can easily understand how the main aim of the 1977 article (Ramfjord, 1977) was to provide some clinical data regarding the performance of the modified Widman flap compared to subgingival instrumentation and pocket elimination, not to propose a further modified version of the procedure!
Just to make you really get the greatness of this renowned Scientist, at the time clinical research was nothing like how we perform it nowadays: in fact, most of the information that we can gather regarding historical flaps is mainly a description of the technique. Therefore, proposing a technique and comparing it to other procedures was a giant leap forward for the time! We also must acknowledge that, in complete honesty, the “modified” modified Widman flap was created through pure Serendipidity: he found something while he was actually looking for something else! (given the wonderful time of the year that we are in, I am dropping you a hint for what will probably be the schmaltziest movie, but an absolute must, of your Christmas Holidays: Serendipidity).
But getting back on track…
How did they do it?- The technique
The “modified” modified Widman flap and its previous version differ for the incisions performed in the aesthetic area. In particular, the 1974 flap design comprehended two incisions in the frontal area: the first one intrasulcular or at the level of the free gingival margin, and the second one at crestal level (Figure 2B, blue arrow). On the other hand, the modification proposed by Ramfjord in 1977 encompassed only one crestal incision in aesthetic cases of the frontal area (Figure 2B, yellow arrow). The execution of just one crestal incision, as opposed to the two incisions included in the modified Widman flap, minimized the post-operatory gingival shrinkage, hence implementing the result where “esthetic considerations are of great importance”, as our dear friend Ramfjord would say.
Then, What all the fuss is about?- The controversy
The “modified” modified Widman flap would have been a wonderful discovery which, you must admit, you were never told of in such a romantic jargon, if not for the fact that it slowly wrote its own obituary (oops, plot twist). Indeed, the shift towards the execution of only one crestal incision in the frontal area made the twice-modified Widman flap absolutely similar to another flap proposed 40 years before and already a celebrity among Periodontists, the Kirkland’s access flap (yes, the most famous of the twins).
During the 80s and the 90s, the most brilliant minds in clinical research were busy performing all the classical longitudinal studies that made the history of Periodontology, such as Ramfjord et al. 1987, Lindhe et al. 1982, Kaldahl et al. 1996 etc. (at their very mention, I know I’m sending you shivers down your spine…).
Well, all these studies compared the long-term performance of the modified Widman flap with non-surgical subgingival instrumentation (Lindhe et al., 1982), and sometimes with Pocket elimination surgery (Ramfjord et al., 1987) or flap and osseous surgery (Kaldahl et al., 1996).In a nutshell, these studies were saying that the twice-modified Widman flap performed better in the long run in terms of Clinical Attachment Level gain and reduction of gingival recession compared to the other previously-mentioned techniques, whenever there was a deep pocket at baseline. But since the twice-modified Widman flap was performed the same as Kirkland’s access flap in the frontal area, what were these studies actually investigating?? Ramfjord’s or Kirkland’s technique?? Well, this controversy raged across Europe and the whole world for decades but no one ever dared to have the last word on the matter (and we are not doing it today… Come on, it’s Christmas!)
So really, what do we know about it?
Of course, it goes without saying that the modified-modified Widman flap was, and probably still is, mistaken for the Kirkland’s access flap. All this controversy of who did it first and which flap all those studies referred to slowly made it fall into disuse (I can clearly feel your disappointment after reading this).
And just how it works for everything, when “two dogs strive for a bone, the third runs away with it” (please allow me the idiom): in fact, regeneration techniques and papilla preservation flaps swept all Periodontists worldwide off their feet, thus changing the approach to periodontal surgery for good. As a consequence, the current indications for the modified Widman procedure (it’s on you to decide which version) are limited to those cases where you need a minimally resective approach. For example, if you have a patient with residual pockets associated with excessive hypertrophic papilla tissues and suprabony defects, the Modified Widman flap procedure would be the perfect fit… and then you must acknowledge how lucky you were to stumble upon this column of the Herald!
See you in the next issue!
Literature and suggested reads
Everett, F. G., Waerhaug, J., & Widman, A. (1971). Leonard Widman: surgical treatment of pyorrhea alveolaris. Journal of Periodontology, 42(9), 571–579. https://doi.org/10.1902/jop.1971.42.9.571
Friedman, N. (1962). Mucogingival Surgery: The Apically Repositioned Flap. The Journal of Periodontology, 33(4), 328–340. https://doi.org/10.1902/jop.1962.33.4.328
Kaldahl, W. B., Kalkwarf, K. L., Patil, K. D., Molvar, M. P., & Dyer, J. K. (1996). Long-term evaluation of periodontal therapy: I. Response to 4 therapeutic modalities. Journal of Periodontology, 67(2), 93–102. https://doi.org/10.1902/jop.1996.67.2.93
Lindhe, J., Westfelt, E., Nyman, S., Socransky, S. S., Heijl, L., & Bratthall, G. (1982). Healing following surgical/non-surgical treatment of periodontal disease. A clinical study. Journal of Clinical Periodontology, 9(2), 115–128. https://doi.org/10.1111/j.1600-051x.1982.tb01227.x
Ramfjord, S. P. (1977). Present status of the modified Widman flap procedure. Journal of Periodontology, 48(9), 558–565. https://doi.org/10.1902/jop.1977.48.9.558
Ramfjord, S. P., Caffesse, R. G., Morrison, E. C., Hill, R. W., Kerry, G. J., Appleberry, E. A., Nissle, R. R., & Stults, D. L. (1987). 4 modalities of periodontal treatment compared over 5 years. Journal of Clinical Periodontology, 14(8), 445–452. https://doi.org/10.1111/j.1600-051x.1987.tb02249.x
Ramfjord, S. P., & Nissle, R. R. (1974). The modified widman flap. Journal of Periodontology, 45(8), 601–607. https://doi.org/10.1902/jop.1974.45.8.2.601
