Women in Implantology - December 10, 2021
Adela Laverick from WIN UK&Ireland is the first of the remarkable women I will be interviewing for the issues of Periocampus Herald. Our WIN Core Group members will also be presenting a case report from their own clinical practice. In this issue, Adela reminds us with her presented case of the potential value of saving natural teeth when we aim for the most favourable dental health outcomes.
In this issue of the Periocampus Herald, I am pleased to launch a series of cases shared by WIN Core Group Members from around the world. I will be presenting a glimpse into the lives of each of these remarkable women, their passions and why they joined WIN. Following the introduction, an interview, the Core Group member will share a patient case to show us what they do in their daily clinical life and why they choose only to offer quality treatments, knowing that this will lead to a satisfied patient over time.
The first lady and colleague I had the honour to interview was Adela Laverick (WIN UK&Ireland). She is a specialist in Prosthodontics and works as an associate in private practice in Perthshire, Scotland. When we talked, she explained to me that being a specialist has opened many doors for her and given her opportunities that she would have missed out on had she remained a general dentist. ‘Being a specialist has allowed me to work with some gifted colleagues in excellent clinics and has helped me to develop my career in implant dentistry,’ she adds. Adela feels privileged to be part of the patient’s journey when they are getting involved with implants. Treating patients with implants, if possible, often results in an improved quality of life, for which the patient is very grateful. When I ask her about how she maintains a healthy work-life balance, she tells me she has been working part-time for many years and believes that this has been key for her: ‘This gives me not just the time, but also the energy to engage fully with both work and life outside of work, such as reading, gardening, walking.’
Talking about why she wanted to be part of WIN: ‘I really enjoy my career, so much that I feel driven to inspire other women into the field, so that more women can enjoy the challenges and rewards of implant dentistry and, in turn, benefit their patients.’ Adela is fully conscious that it is important that young female dentists are educated about implant dentistry as a career option and that there are visible female role models out there to inspire them. And, last but not least, I asked her about the future WIN UK&Ireland plans, and she shared with me that the focus will be on three themes: raising awareness, providing support, and providing education, with the overall aim of engaging more women!
Sounds fantastic, Adela, thank you so much—and let’s all enjoy now the case Adela decided to share with us; have a great read!
Case Report
Demonstrating the potential advantages of saving natural teeth
In the era of successful implant treatment, it is easy to decide to extract teeth and replace them with implants. However, implant treatment is not without problems, and it is widely acknowledged that such treatment can be associated with both biological and mechanical complications. This case report and the cited literature have been chosen to remind us of the potential value of saving natural teeth when we aim for the most favourable dental health outcomes.
BRIEF PATIENT HISTORY:
A 72-year-old female patient, PM, attended our clinic in March 2013.
Her complaints were that she was struggling to wear her partial dentures and also that her teeth were beginning to fail, with repeated loss of crowns and some loose teeth. She wished to have a more comfortable and functional replacement for her teeth.
Socially she was part of a choir and felt that her poor teeth were beginning to affect her singing. Medically she took the diuretic bendroflumethiazide for mild hypertension and was otherwise healthy.
INITIAL EXAMINATION confirmed the following:
- Partially dentate patient
- All maxillary teeth were heavily restored and showing signs of biological or structural failure
- Generalised periodontal inflammation with associated mobility of several teeth
TREATMENT PROVIDED:
STAGE 1: Removal of active disease
- The initial phase of periodontal treatment with the hygienist
- Extraction of all failing upper teeth and fitting of immediate maxillary provisional complete acrylic denture
STAGE 2: Reassessment
- Assessment of oral hygiene and periodontal health around remaining mandibular teeth
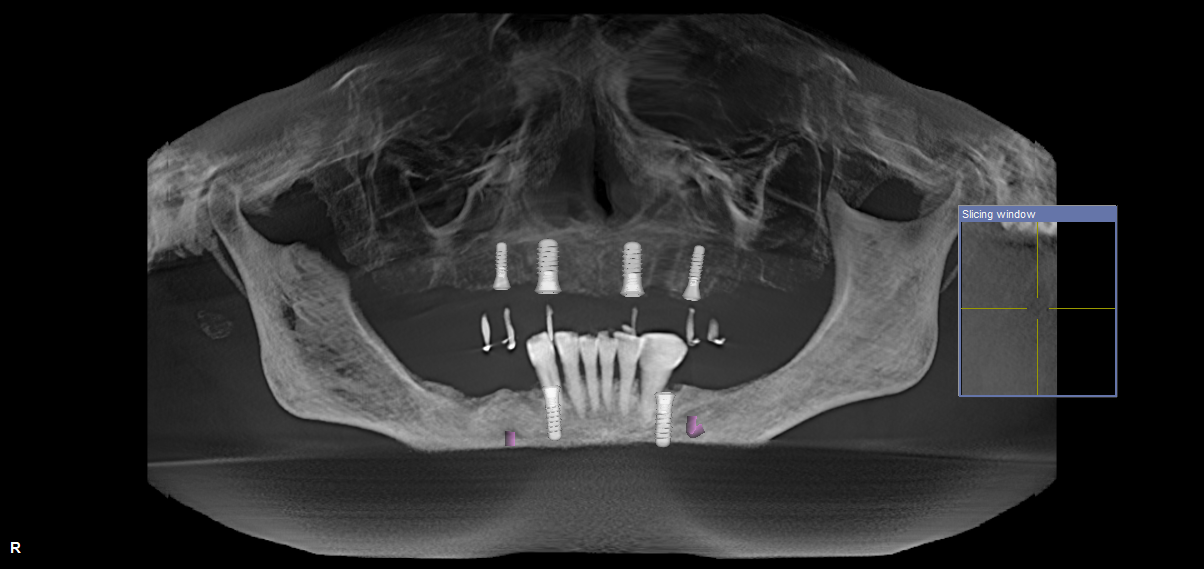
- 3D CT scan
- Discussion of treatment options
At this stage, Mrs. PM had six remaining teeth: 31, 32, 33, 41, 42, 43. Both canines were mobile, with a significant loss of periodontal bone support. However, the mandibular incisors were periodontally stable and had minimal mobility, and Mrs. PM was maintaining an excellent standard of oral hygiene. We, therefore, discussed the option of keeping these four remaining natural teeth and designing the prosthesis around them. Mrs. PM was very keen to keep her teeth and seemed to take some psychological and emotional comfort from being able to do so.
The scan was assessed for available bone volume, and the following treatment plan was agreed upon:
Maxilla: restore with four implants, locator abutments and a horseshoe overdenture.
Mandible: place two implants, one on either side of the remaining natural teeth, to help to stabilise and retain a mandibular partial overdenture.
STAGE 3: Placement of implants
- September 2013: placement of maxillary implants at sites: 12,14,22,24; all were Straumann tissue level Standard Plus (SP) Regular neck (RN) implants
- October 2013: placement of mandibular implants at sites 33 and 43; both were Straumann tissue level Standard RN implants
STAGE 4: Restorative phase
- The maxilla was restored with an overdenture on four locator abutments
- The overdenture was a horseshoe design with a cobalt-chromium palate
- Care was taken to refer to previous photos for tooth shape, size and position to achieve a natural appearance
- The lower arch was restored with a very simple partial overdenture: two acrylic saddles linked by a lingual bar, retained and stabilised by locator abutments on the two implants
STAGE 5: Review and long-term maintenance
- Mrs. PM adapted very quickly to the new prostheses and, at her initial review, shared that she was comfortable and happy with their appearance and that both of the overdentures ‘felt snug’
- She has been reviewed annually since and was last seen in August 2020
- Both of the original overdentures are still functioning well
- Two of the maxillary locator abutments were replaced because of excessive wear
- Otherwise, there has been minimal intervention: replacement of the retentive inserts when necessary
- Interestingly, the mandibular partial overdenture has been extremely stable and only rarely has needed to have the inserts replaced
DISCUSSION POINTS
Retaining natural teeth:
This case highlights the importance of retaining natural teeth where possible. With only 4 viable natural teeth remaining, it would have been very easy to recommend extracting these teeth. However, it was evident that Mrs. PM gained significant psychological benefit from being able to retain at least some of her own teeth, and she has also benefited from the protective proprioception that natural teeth provide. In addition, the mandibular partial overdenture is very stable and does not have the anteroposterior rock that, in my experience, is often seen with complete mandibular overdentures supported by two locators. The natural teeth provide indirect retention and contribute to the stability of the restoration.
A paper by Clark and Levin (2019) asks, ‘In the dental implant era, why do we still bother saving teeth?’ In this paper, the authors remind us that teeth are vital sensory organs that are associated with quality of life and contribute to speech, function and smiling. The authors also ask, do our patients undervalue teeth and their preservation? In my experience, many patients incorrectly believe that implants are better than teeth, rather than understanding that well-executed implant treatment is an excellent treatment modality for teeth that have failed.
Pjetursson and Heimisdottir (2018) ask, are dental implants better than teeth? The authors remind us that dental implants' survival and success rates will never succeed the survival rates of healthy, clean teeth and that dental implant treatment is associated with a risk of biological and technical complications.
When considering whether or not to save teeth, it is essential to remember that treatments to save compromised teeth—such as endodontics and periodontal treatment—have similar success rates to implants, but more importantly, these treatments retain the natural tooth for longer. When planning treatment for our patients, it is critical to remember that extraction is irreversible and that retaining a natural tooth can have multiple benefits for our patients, including limiting the psychological effects of tooth loss.
Design of the partial overdenture:
A key aspect in the planning of this case was that it was necessary to have adequate space between the implant abutment and the remaining natural teeth for the overdenture housing and adequate acrylic to retain it within the prostheses. Therefore, the 3D positioning of the implant was as important as in a fixed restorative case.
In this particular case, the design of the partial overdenture was kept extremely simple, with the two saddles being linked by a simple lingual bar. This simple design served to minimise coverage of the gingival margins, which is particularly desirable in a patient with a history of periodontal disease.


 |
 |
Literature and recommended reads:
Clark, D., & Levin, L. (2019). In the dental implant era, why do we still bother saving teeth? Dental Traumatology, 35(6), 368–75. https://onlinelibrary.wiley.com/doi/full/10.1111/edt.12492
Pjeturrson, B.E., & Heimisdottir, K. (2018). Dental implants – are they better than natural teeth? European Journal of Oral Sciences, 126(Suppl):81–87. https://onlinelibrary.wiley.com/doi/full/10.1111/eos.12543
