Exploring Communication - February 21, 2020
Words really do matter …
The realm of communication and behaviour change in dentistry has evolved to be a topic of huge interest. This has hence led me to further explore the power of the words we use within dentistry, to communicate to patients and amongst the profession. Behaviour change tools can be highly effective in supporting behaviour change within patients’ oral health and their commitment to their oral care. Despite this being an area that is supported by extensive evidence-based behavioural change models (Ramseier & Suvan, 2010), there seems to be less supporting evidence in dentistry that focuses on the choice of the words we use to communicate to our patients.
This article explores the supporting evidence for non-surgical periodontal therapy, followed by a discussion on the relevance of the words ‘scale and polish’, ‘cleaning’ and ‘clean’. These words are renowned for being associated with dental hygiene appointments and how this fits into the evidence supporting non-surgical periodontal therapy. Some clinicians have already implemented changes in their choices of the words they use. Despite this being the case it would still appear that the majority of clinicians continue to be in dental settings where ‘scale and polish’, ‘cleaning’ or ‘clean’ seem to be some of the most common terms used relating to hygiene treatments.
The evidence supporting routine scale and polish for periodontal health in adults
In summary, a recent Cochrane report published in December 2018 included 1711 participants (Lamont, Worthington, Clarkson, & Beirne, 2018). The author stated that in adults without severe periodontitis, regular attenders at the dental practice, with routine scale and polishes, the treatment makes little or no difference to their gingivitis, probing depths or the quality of life over a 2-3 year follow-up period. There was also little or no difference in the plaque levels over these two years. Despite a reduction of calculus with scale and polish appointments every 6 months over a 2-3 year period, the clinical importance of these small reductions was uncertain.
From this Cochrane report, a scale and polish appointment would appear to be up for debate and challenged considering there was no improvement in gingivitis, probing depths, quality of life or plaque levels.
If supra and subgingival plaque and calculus removal takes place with hand and powered instruments, this done alone does not reduce gingivitis, as demonstrated in Needleman’s research in 2015 (Needleman, Nibali, & Di Iorio, 2015).
The evidence would suggest the standard name ‘scale and polish’, ‘cleaning’ or ‘clean’ given to hygiene treatments and the approach to treating gingivitis needs to be challenged. The focus needs to be on the obvious - oral hygiene. Hygienists and Dental Therapists are fully aware of the time required and needed for oral hygiene instruction, along with the implementation of effective behaviour change models and results.
Another study focused on the patients’ views on periodontal disease; attitudes to oral health and expectation of periodontal treatment’ (Abrahamsson, Wennström, & Hallberg, 2008). The study was essentially an interview format asking patients about how they felt about their diagnosis prior to treatment. In the results, patients felt they had a low degree of control over treatment, decisions and treatment outcomes. In conclusion, a degree of vulnerability after patients’ diagnosis was identified with an emphasis on the need for the importance of communication in dentistry.
It is widely accepted that a preventative program that stimulates patients to adhere to proper oral hygiene habits are likely to resolve gingivitis and prevent the progression of periodontal disease (Axelsson & Lindhe, 1978).
Hygienists and Dental Therapists and communication
It is widely accepted that Hygienists and Dental Therapists are renowned for their communication skills within oral health and within the dental team. The value of the Hygiene department cannot be underestimated for the crucial role played in engaging patients with their oral health. Despite this, there continue to be areas within communication to support the improvement of oral health that can be enhanced. The implementation of evidence-based behaviour change models is certainly successful.
Challenging the words used that support an oral hygiene focused appointment
The potential engagement in oral health will undoubtedly be affected by sub-optimal communication and the words that can truly communicate the intentions of the results we wish to achieve.
If the dental profession and dental team as a whole were to universally change the words ‘scale and polish’ and ‘cleaning’ or ‘clean’ to other words more pertinent to the hygiene treatment, is this likely to impact the patients’ perception and expectation of an appointment in a different way? It may be accepted that the words ‘scale’ and ‘polish’ are currently being misused.
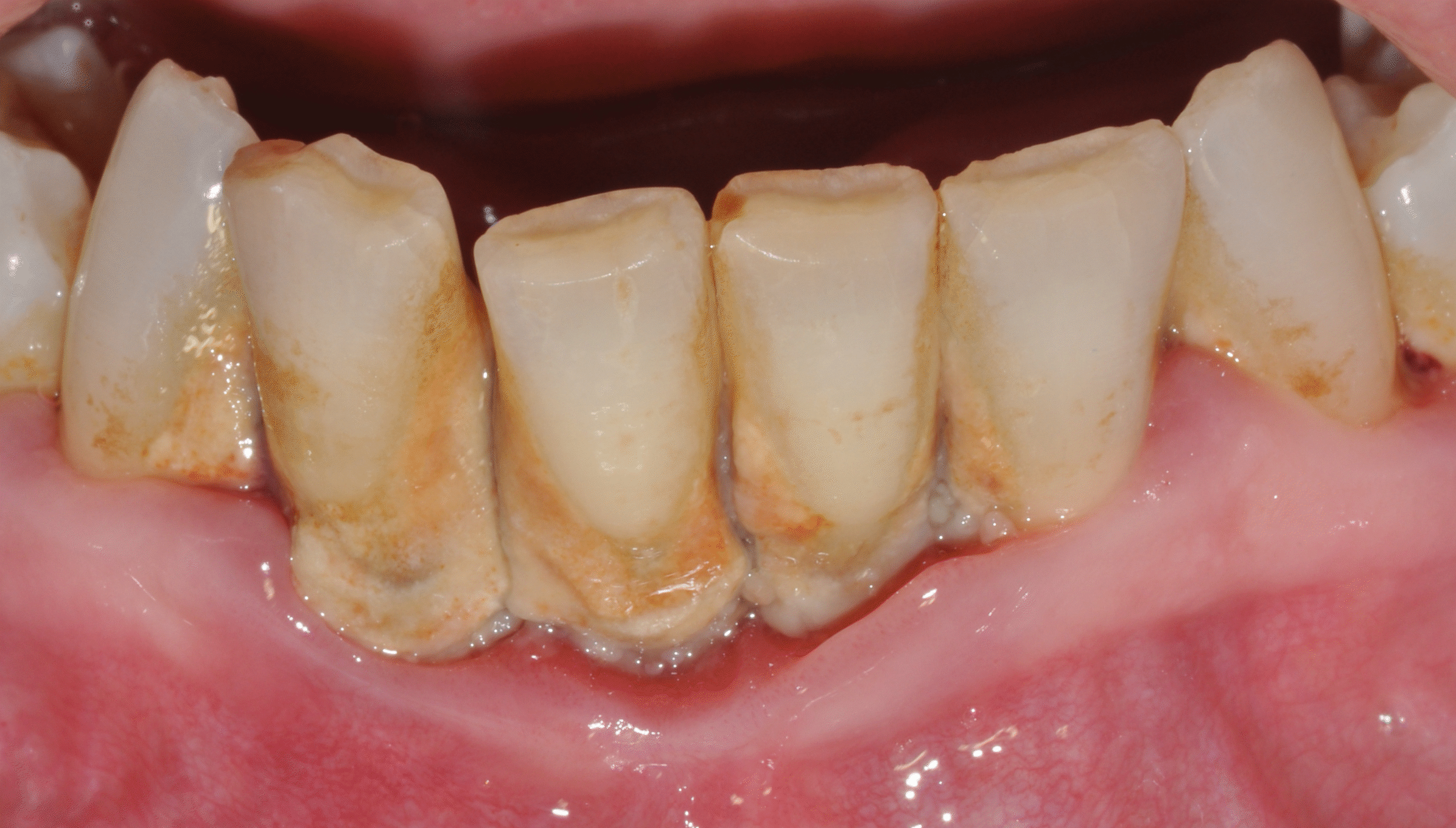
Patients perceive it too often be a cosmetic treatment, requesting a polish. This is not the focus of the treatment, we are treating a disease. (Clinical pictures courtesy of Prof. Filippo Graziani)
What does a ‘scale and polish’ or a ‘cleaning’ or a ‘clean’ really mean to the patients?
The choice of words is critically important if we wish to convey a clear message to the patients.
Are the words a true reflection of the meaning of the appointment? In other words were adopted throughout the dental team, to describe the purpose of the treatment, could treatment outcomes be affected in the long term? Would patients be more at ease and accepting to actively talk about oral hygiene for an appointment? If patients were prepped accordingly by all members of the team and they had not been told they needed to be booked for a scale and polish, cleaning or clean how could treatment outcomes be different?
What we say, and how we say it, is significant in the communication to the patients’ understanding of the significance of periodontal disease.
On speaking to a handful of colleagues that have been qualified on average over 10 years, from posting on social media, the below feedback was sent. I received a variety of responses all in agreement that scale and polish, cleaning and clean do not support successful treatment outcomes, due to the varied challenges these words bring and are potentially having a negative impact on our roles and delivery of treatment.
The below are just a few summaries of the consequences mentioned in the responses received:
- Patients clock-watching, intent on receiving the full scale and polish as that is what they booked for.
- Prioritising a polish over the health of their gums or acceptance of the disease.
- Dissatisfied if they do not get what they consider to be the full scale and polish that they have been booked in for.
- Patients are expecting a scale and polish and can become agitated when they don’t get this.
- It makes delivering oral hygiene more challenging to deliver for one appointment if the appointment has been labelled a scale and polish, or it is ingrained in the patients’ head that they are attending a hygiene appointment for a scale and polish.
- A polish is infrequently indicated and it makes it challenging when it is not carried out.
- For years select polishing has been used although the term scale and polish does not reflect this.
- Patients perceive it to often be a cosmetic treatment, requesting a polish. This is not the focus of the treatment, we are treating a disease.
- ‘I’m here just for a clean’. Which undervalues the complexity and value of our role.
- Social media campaigns don’t help either. Adverts for things like charcoal toothpaste drive demand for quick cleans and immediate results and give the impression there’s nothing to it.
Despite feedback being received on these words some hygienists and dental therapists do already use other words to describe their hygiene treatments.
Change will continue to take place as we refine our skillset to continuously improve.
Based on the content of this article so far. Options of new words to use are suggested below: |
|---|
|
These are mere suggestions open for debate, but by changing the words the meaning of the appointment changes. If all members of the team communicate the new choice of words, over time it is likely to be possible to change the patients’ perception and expectations of the appointment.
Ultimately the pressure to perform a scale and polish is no longer there as the appropriate treatment required for that patient becomes the focus rather than being dictated by the appointment name.
For the purpose of this article and on reflection of the Cochrane review referred to, the results did not justify a scale and polish. These could arguably be strong enough grounds to support the implementation of new words to describe a hygiene appointment and what is carried out within the hygiene appointment.
The evidence potentially supports a revision for the sake of the patient to be more accepting of an appointment focussed on oral hygiene especially when a Cochrane review including 1711 patients does not support a scale and polish. It is also important to consider how patients felt in the study referenced previously with a low degree of control over treatment, decisions and treatment outcomes. If patients realised they do have a higher degree of control if they take charge of their oral hygiene affecting the treatment outcomes their attitudes could change.
As with every part of one's professional career path as it evolves it is our responsibility and commitment to learn more that furthers the profession. It is important to never underestimate the value of the instruments we use.
Conclusion
From exploring the evidence supporting the scale and polish treatment, additional actions need to be taken to change treatment modalities. From supporting papers that have been included in this article, it seems the correct time to introduce the terms to accurately communicate treatments. These terms need to be adopted by the whole team to successfully increase the patients’ perception and expectation of hygiene treatment.
Refining the choice of words used could be explored further, and additional articles on the psychology of chosen words within medicine and dentistry need to be explored further. There are significant areas of research that could potentially be carried out around this subject matter.
As science and technology change, so should the way in which we educate and motivate our patients through the spoken word.
Literature and suggested reads:
Abrahamsson, K. H., Wennström, J. L., & Hallberg, U. (2008). Patients’ views on periodontal disease; attitudes to oral health and expectancy of periodontal treatment: a qualitative interview study. Oral Health & Preventive Dentistry, 6(3), 209–216. http://www.ncbi.nlm.nih.gov/pubmed/19119575
Axelsson, P., & Lindhe, J. (1978). Effect of controlled oral hygiene procedures on caries and periodontal disease in adults. Journal of Clinical Periodontology, 5(2), 133–151. https://www.ncbi.nlm.nih.gov/pubmed/275282
Lamont, T., Worthington, H. V., Clarkson, J. E., & Beirne, P. V. (2018). Routine scale and polish for periodontal health in adults. Cochrane Database of Systematic Reviews, 2018(12). https://www.ncbi.nlm.nih.gov/pubmed/24197669
Needleman, I., Nibali, L., & Di Iorio, A. (2015). Professional mechanical plaque removal for prevention of periodontal diseases in adults--systematic review update. Journal of Clinical Periodontology, 42 Suppl 16:S12-35. https://www.ncbi.nlm.nih.gov/pubmed/25495962
Ramseier, C. A., & Suvan, J. E. (Eds.). (2010). Health Behavior Change in the Dental Practice. Ames, Iowa USA: Blackwell Publishing, Inc. https://onlinelibrary.wiley.com/doi/book/10.1002/9781118786802
