Perio arena - November 05, 2020
When the objective is to modify the periodontal phenotype (as in this case), there is no other technique than split-thickness non-advanced tunnel able to achieve the same results in the short term. A good periodontist needs to know and to control all the evidence-supported techniques and be able to take advantage of each of them, depending on the specific characteristics/objectives of the case.
A 46 years old woman was referred to the Master in Periodontology at Complutense University of Madrid worried about the self-perceived esthetic appearance of her lower teeth, associated with dentinal hypersensitivity and discomfort during brushing. After the clinical evaluation, the following periodontal diagnosis was elaborated:
- Gingival inflammation in periodontitis patient;
- Multiple gingival recessions affecting teeth 43-44-45.
According to this diagnosis, the patient received non-traumatic oral hygiene instructions, full-mouth scaling and oral hygiene compliance re-evaluation at 2 weeks.
At the re-evaluation, in accordance with the patient’s request, a root coverage procedure was planned in the IV sextant. From 43 to 45, three RT1/RT2 gingival recessions of 2 to 4 mm were present (Figure 1). The gingival margin was thin, and the amount of keratinised tissue (KT) was less than 2 mm on 44-45.
Treatment goals
The treatment goals were to:
- Obtain complete root coverage of all the gingival recessions of the involved teeth;
- Improve self-perceived patient aesthetics;
- Reduce the dentinal hypersensitivity;
- Increase the KT width;
- Augment the tissue thickness.
Chosen surgical approach: split-thickness non-advanced tunnel
According to the treatment goals, a split-thickness non-advanced tunnel (Zabalegui et al. 1999) was planned. Indeed, one of the main objectives of the procedure was the short-term modification of the periodontal phenotype. However, while most of the other available techniques (e.g. coronally advanced flap (CAF) or modified coronally advanced tunnel) can achieve a postoperative increase in tissue thickness when associated with the use of a CTG, the increase in KT width is generally obtained only in the long term as a consequence of the re-alignment of the mucogingival junction (Rasperini et al. 2018).
Tunnel procedures have first been described by Allen et al. (1994), in order to treat up to two adjacent gingival recessions. A further development of this technique was proposed to treat several adjacent gingival recessions by Zabalegui et al. (1999). This technique is based on the use of a connective tissue graft (CTG) placed inside a partial-thickness (supraperiosteal) bed, and partially leaving the CTG exposed during healing. The survival of the exposed graft is expected due to the double layer of vascular supply by the internal layer (periosteum) and by the external layer within the tunnel. This surgical approach (supraperiosteal tunnel) has shown clinical efficacy in the root coverage of multiple adjacent gingival recessions, as well as an increase of the width of keratinised tissue (Zabalegui et al. 1999; Tavelli et al. 2018).

Description of the surgical procedure
After local anaesthesia, a split-thickness bed was prepared at the involved teeth on a single plane, far beyond the mucogingival line, using an ophthalmic micro-blade. This bed was started on top of the gingival margin and extended laterally up to reach a plane extended 5 mm in all directions from the mucosal margin of the involved teeth and undermining the facial surface of the interdental papillae, to a position 2 mm coronal to the CEJ (Figure 2). Special attention was paid to avoid disrupting the interdental papillae or perforating the flap. The exposed teeth surfaces were then decontaminated utilising an ultrasonic device.

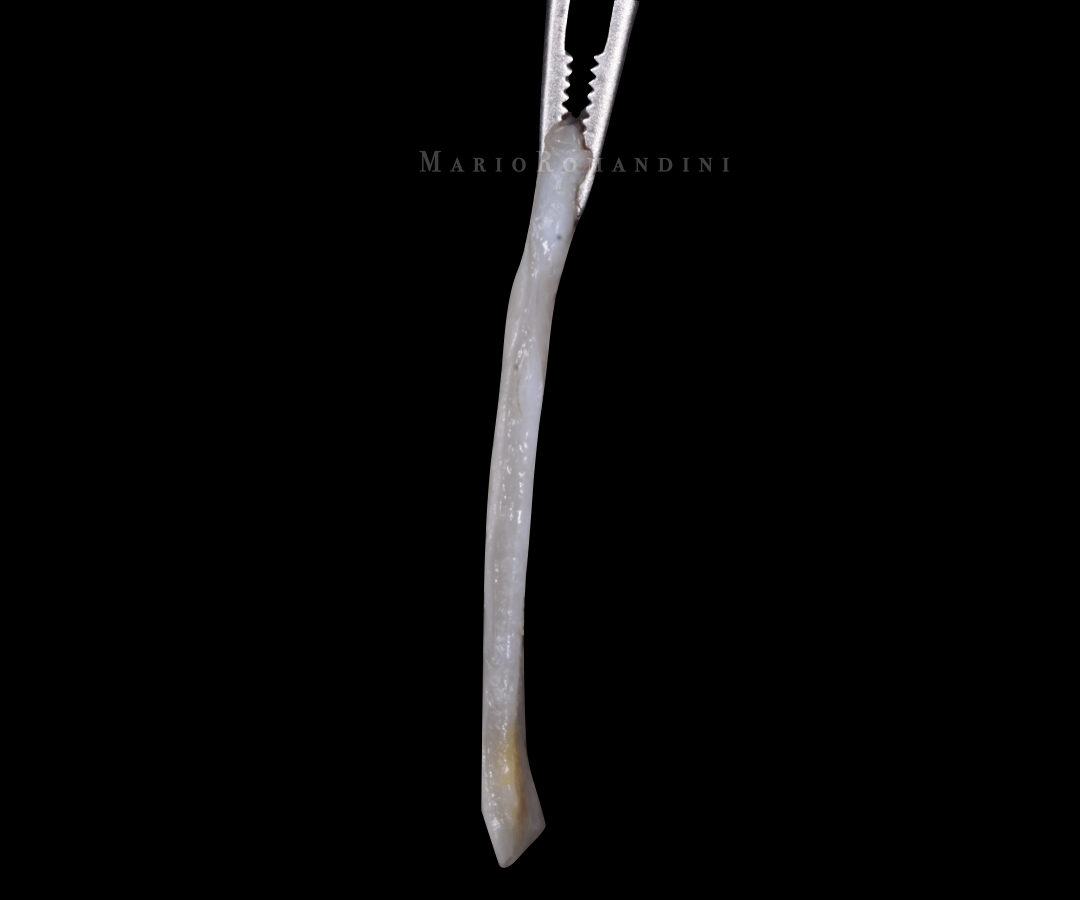
A free gingival graft (1.5 mm thickness, extending 3 mm in all directions from all the gingival margins of the involved teeth) was then harvested from the palate and de-epithelialised (Figure 3). The donor site was sutured with tooth-suspended cross-mattress horizontal sutures.
The connective tissue graft (CTG) was then placed into the split-thickness bed and sutured. Two sutures were placed, one at the most mesial, and the other at the most distal aspect of the tunnel, positioned in a way to allow the correct corono-apical position of the CTG (its coronal part slightly coronal to the level of the CEJ). The CTG was pushed inside the tunnel through the most central recession (Figure 4).

The insertion was facilitated pushing it with a tunnelling instrument and pulling it by the sutures at the same time, with the help of the dental assistant. No attempts were made to advance the tunnel. Consequently, thanks to the split-thickness bed preparation, a part of the graft was intentionally left exposed (Figures 5-6).


After positioning the CTG, the site was rinsed with saline solution to remove any clot. Mild compression with a sterile gauze with saline was carried out for 10 minutes after completing the surgical procedure.
Postoperative care
Postoperatively, the patient was instructed to stop any mechanical self-performed oral hygiene procedure in the surgical area for 2 weeks after the surgery and to rinse for 1 min with 0.12% chlorhexidine + 0.05 CPC 3x/day for 4 weeks. She then started to brush the operated zone with a surgical toothbrush for another 2 weeks, and at 1 month she resumed a conventional a-traumatic mechanical self-performed oral hygiene procedure.
The patient was also instructed to avoid any trauma on the surgical zone (e.g. eating hard food), and not to make any sport activity until suture removal.
The sutures of the palatal donor site were removed 7 days after surgery, while the sutures of the receiving zone were removed at 14 days.
Clinical outcomes
At the 8-months follow-up (Figure 7), complete root coverage was present on all the treated teeth; the patient was satisfied with the aesthetic appearance of the treated zone and reported no dentinal hypersensitivity. The desired increase in KT width and soft tissue volume was also observed. With that, all the pre-treatment goals were accomplished.

Technical tips
- Being one of the most technically-sensitive procedures of periodontology, a split-thickness non-advanced tunnel is more successful when performed with the use of micro-surgical instruments (e.g. ophthalmic micro-blades) and adequate magnification.
- This case was part of a clinical study: consequently, according to the protocol, a de-epithelialised CTG was used. However, with this technique, a sub-epithelial connective tissue graft (e.g. Huerzeler & Weng 1999) is to be preferred to facilitate the vascularisation of the exposed graft and to reduce the occurrence of postoperative scars.
- In few cases, particularly if a de-epithelialised CTG is used, or if the micro-blade is inserted in the sulcus (and not into the top of the gingival margin), postoperative scars may appear between the exposed graft and the gingival margin. In those cases, a diamond bur can be used after healing - as it was done in this case - to de-epithelialise the scars, thus improving the final aesthetic result.
- Every single step is crucial to obtain complete root coverage with this technique. Everything can be perfectly done and then ruined with the last step: suturing! It is imperative that the CTG is secured in a position slightly coronal to the CEJ. To achieve this, the split-thickness bed (undermining the papillae) needs to be prepared very carefully and to realise the suturing technique adequately.
Conclusions
We are Italians, we all like CAF. And as one of the Italians, I love CAF too. However, a good periodontist needs to know and to control all the evidence-supported techniques and be able to take advantage of each of them, depending on the specific characteristics/objectives of the case. I had the privilege to learn this technique directly from the Master who described it in 1999: Ion Zabalegui. I will always be grateful to this great clinician, dedicated professor and special man.
This technique requires training, as it is a very technically-sensitive procedure. However, at least when the objective is to modify the periodontal phenotype (as in this case), there is no other technique able to achieve the same results in the short term. I encourage you all to use it!
Literature and suggested reads:
Allen, A. L. (1994). Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. The International Journal of Periodontics & Restorative Dentistry, 14(3), 216–227. https://pubmed.ncbi.nlm.nih.gov/7995692/
Hürzeler, M. B., & Weng, D. (1999). A single-incision technique to harvest subepithelial connective tissue grafts from the palate. The International Journal of Periodontics & Restorative Dentistry, 19(3), 279–287. https://pubmed.ncbi.nlm.nih.gov/10635174/
Rasperini, G., Acunzo, R., Pellegrini, G., Pagni, G., Tonetti, M., Pini Prato, G. P., & Cortellini, P. (2018). Predictor factors for long-term outcomes stability of coronally advanced flap with or without connective tissue graft in the treatment of single maxillary gingival recessions: 9 years results of a randomised controlled clinical trial. Journal of Clinical Periodontology, 45(9), 1107–1117. https://doi.org/10.1111/jcpe.12932
Tavelli, L., Barootchi, S., Nguyen, T. V. N., Tattan, M., Ravidà, A., & Wang, H.-L. (2018). Efficacy of tunnel technique in the treatment of localised and multiple gingival recessions: A systematic review and meta-analysis. Journal of Periodontology, 89(9), 1075–1090. https://doi.org/10.1002/JPER.18-0066
Zabalegui, I., Sicilia, A., Cambra, J., Gil, J., & Sanz, M. (1999). Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: A clinical report. The International Journal of Periodontics & Restorative Dentistry, 19(2), 199–206. https://pubmed.ncbi.nlm.nih.gov/10635186/
